Adenosine Triphosphate (ATP) plays a critical role in various cellular functions, including those related to diabetes. Here’s how ATP is involved in diabetes:
- Energy Production and Glucose Metabolism
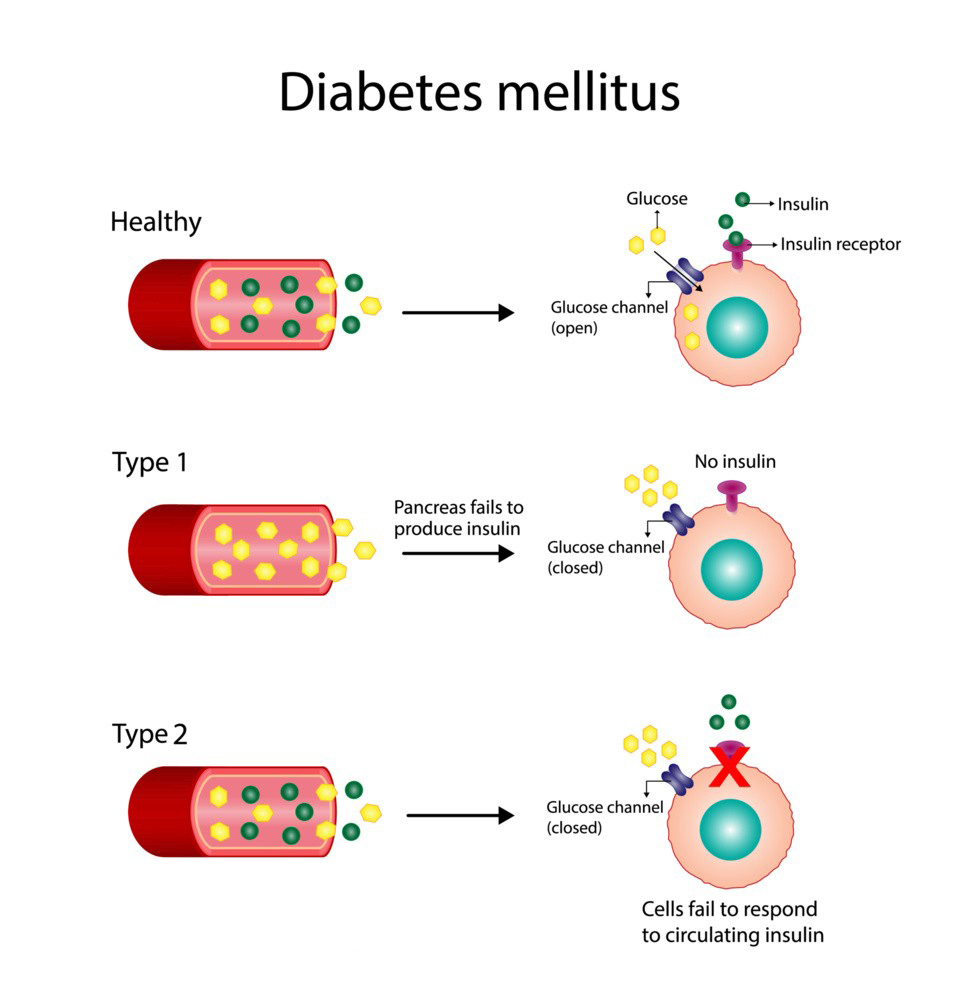
Adenosine Triphosphate is the primary energy currency of cells. In diabetes, particularly type 2 diabetes, the body’s ability to regulate glucose is impaired, leading to insulin resistance. Insulin is responsible for allowing glucose to enter cells, where it is used for energy production via Adenosine Triphosphate. When insulin signaling is defective, cells become less efficient at producing ATP, contributing to high blood glucose levels and cellular energy deficits.
In healthy individuals, Adenosine Triphosphate is generated during glycolysis and oxidative phosphorylation. However, in diabetes, mitochondrial dysfunction may occur, impairing ATP production and disrupting glucose metabolism.
2. Adenosine Triphosphate and Insulin Secretion
In type 2 diabetes, the pancreas struggles to produce enough insulin. Adenosine Triphosphate plays a crucial role in insulin secretion from pancreatic β-cells. When blood glucose levels rise, glucose enters β-cells and is metabolized to produce ATP. The increase in Adenosine Triphosphate levels leads to the closure of ATP-sensitive potassium (K_ATP) channels, which causes depolarization of the cell membrane, triggering calcium influx and insulin release. A defect in ATP production or signaling can hinder insulin secretion, exacerbating hyperglycemia.
3. Mitochondrial Dysfunction and Oxidative Stress
Mitochondria are responsible for Adenosine Triphosphate production through oxidative phosphorylation. In both type 1 and type 2 diabetes, mitochondrial dysfunction is a common issue, leading to reduced ATP production. This dysfunction can also contribute to increased oxidative stress, as poorly functioning mitochondria produce more reactive oxygen species (ROS). This oxidative stress can damage cells and tissues, worsening insulin resistance and leading to complications associated with diabetes, such as neuropathy, nephropathy, and retinopathy.
4. Adenosine Triphosphate and Inflammation
Chronic inflammation is a feature of type 2 diabetes, and Adenosine Triphosphate has been found to influence inflammatory pathways. Extracellular Adenosine Triphosphate can act as a signaling molecule that activates purinergic receptors, which are involved in inflammation and immune responses. High levels of extracellular Adenosine Triphosphate may exacerbate inflammation, contributing to insulin resistance and β-cell dysfunction.
5. Adenosine Triphosphate and Diabetes Complications
In diabetes, Adenosine Triphosphate deficits in various tissues can contribute to complications such as diabetic neuropathy, where nerve cells become damaged due to both energy deficits and oxidative stress. Similarly, insufficient Adenosine Triphosphate in endothelial cells lining blood vessels may impair vascular function, leading to cardiovascular complications.
In Summary:
Adenosine Triphosphate is crucial in glucose metabolism, insulin secretion, and cellular energy regulation. Dysfunction in Adenosine Triphosphate production or utilization due to mitochondrial dysfunction, oxidative stress, or impaired insulin signaling is a key factor in the development and progression of both type 1 and type 2 diabetes. Understanding ATP’s role in these processes is important for managing diabetes and potentially developing therapies to address metabolic defects.
